The micriobiome-gut-brain axis
I've thought a lot about what my first blog post should be. I didn’t want it to be something too specific but it needed to give enough depth to be worthy of that 'first post' title.
Something that has really stuck out to me is that, we tend to look at the human body as two entities- neurological function and physiological function, brain and body, mental and physical. But why? Why don’t we question the impact of our mental health on our physical and vice versus.
There is a long history of research into the gut-brain axis and the various complex connections which maintain normal homeostasis (balance) in the body.- This bidirectional communication is maintained through direct and indirect signalling of a number of systems:
Neurological- between the central nervous system (CNS) and enteric nervous system (ENS) and the relay systems the autonomic nervous system (ANS), and vagus nerve,
Immune system- various immune cells and cytokines initiating responses
Endocrine (hormone) system- The hypothalamic- pituitary-adrenal axis (HPA axis) and various gut hormones.
Figure 1: The bidirectional communication of the brain, gut and microbiome. Image adapted from Nature reviews study ‘The gut-microbiota-brain axis in behaviour and brain disorders’ (Mazmanian et al., 2021).
Early research into the gut-brain axis has focused primarily on its role in digestion and satiety; letting your body know that you are eating and to digest the food and vice versus to tell the brain that you are full and to stop eating. However, we have learnt through a number of pathophysiological consequences that the gut-brain connections serves a much greater role in maintaining homeostasis namely through the impact of stress, gut inflammation, and mood/behavioural changes.
The ancient Greek physician, Hippocrates said almost 2500 year ago that- 'all disease begins in the gut'. I don’t think this had really been understood until more recent years, where research has provided evidence to support the significant impact that stress and damage to the intestinal walls has in disease mitigation.
However what really intrigues me about this interaction is the influence the microbiome has on this axis! There have been many recent studies into the impact of microbe depletion in rodents - with significant correlation between microbe depletion and dysfunction in homeostasis in immune function, hormone signalling and neurotransmission.
The microbiome is an ever changing entity of bacterial species that adapt and change throughout our lifetime in response to factors such as stress, diet, age, genetics and changing external environments. Essentially the gut microbiome is the system that lies between the internal and external environment, sensing and receiving signals from our environment and then processing and mediating a response.
Gut bacteria produce a host of different by-products during fermentation and digestion of nutrients in the gut;
Neurotransmitters (e.g. GABA, adrenaline, serotonin- associated with the feeling of happiness and dopamine- associated with the feeling of reward)-
Amino acids,
Vitamins (vitamin K-essential for bone development and blood clotting)
Short chain fatty acids (SCFA).
Short chain fatty acids are particularly important by-products produced through microbiota fermentation of dietary fibre, hence the importance of fibre in the diet. They help to regulate pH, regulate appetite, are a source of energy for the cells of the gut lining (protection), have positive effects on memory and brain function, have anti-inflammatory properties (prevention against cancers) and reduce fat storage. And that is only a few of the properties.
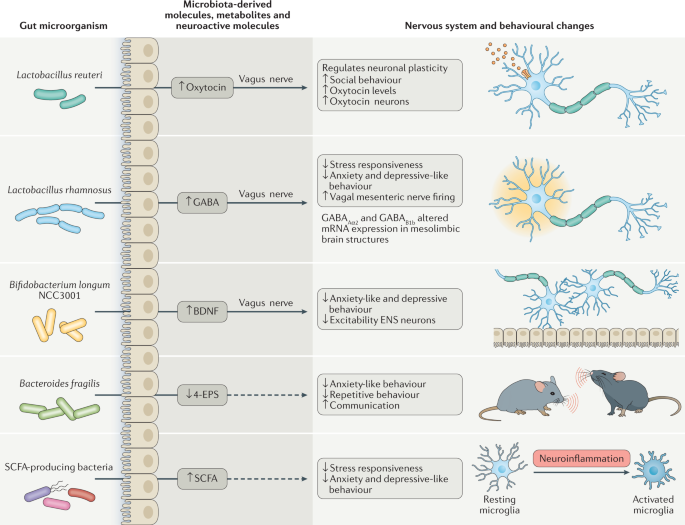
Figure 2: Molecules and metabolites secreted by microbiota in the process of digestion and fermentation and the relative nervous system and behavioural responses they initiate. Image from Nature reviews article ‘The gut-microbiota-brain axis in behaviour and brain disorders’ (Mazmanian et al., 2021).
All of these substances act directly on neurons such as the vagus nerve and ANS which relays messages between the gut and brain or indirectly by travelling through circulation to distant receptors of the body.
Ever wondered why when you feel stressed, you experience symptoms of constipation when stress is a 'mental emotion' ?- well stress can cause microbiome dysbiosis (an imbalance of productive and pathogenic bacteria) and therefore dysfunction in the production of all the metabolites I've just mentioned. Without these metabolites, bowel motility is slowed as the foods we ingest cannot be broken down and utilised as efficiently, leading to symptoms of constipation.
The bidirectional communication of the gut-brain axis and the contribution of the microbiome can be evidenced through a number of studies into illnesses that previously have been characterized by defects in brain function and termed 'mental illnesses'. These include developmental disorders such as autism spectrum disorder, stress disorders such as anxiety and depression disorder and neurodegenerative disorders such as parkinson's and alzheimer's disease.
In ASD individuals, gastrointestinal dysfunction is more prevalent than neurotypical counterparts- individuals experience increased susceptibility to gut inflammation and intestinal permeability.
In patients with Parkinsons, constipation and other gastrointestinal issues are observed in around 80% of cases and the presence of gut inflammation and early accumulation of alpha synuclein protein (a characteristic sign of Parkinsons) in the ENS and vagus nerve suggests that parkinsons may even start in the gut and become a brain pathology through neuronal pathways. Alternatively, in alzheimers some pathogenic bacteria (e.g. shigella spp) are associated with the production of amyloid proteins- a characteristic sign of Alzheimers disease
Finally, Stress disorders anxiety and depression are associated with the failure in allostasis (balance of the stress response systems) and there is strong evidence to highlight that there is a bidirectional connection between stress response and the gut microbiota- gut microbiota can normalise the production of glucocorticoids (stress hormones that produce anti-inflammatory response), maintain allostasis and regulate brain derived neurotropic factor (BDNF) associated with the formation of neurons, learning and memory.
Here, for the purpose of looking into the impact of the gut microbiota on the gut-brain axis, I have given examples of 'mental' illnesses however, the same can be observed for many physical diseases- an individuals mental fitness can influence physical disease.
The research into the gut-brain axis and the potential influence of the gut microbiome provides compelling evidence to highlight that homeostasis depends on the bidirectional communication between both entities through a number of complex signalling pathways- Although, the major signs and symptoms of diseases may present as either mental (stress, anxiety, memory loss, inability to focus) or physical (muscle fatigue, digestion issues, skin problems) this may not be the source of the problem and perhaps considering the human body as one entity may provide new target options for therapy.